In October, two inner official communiqués on bettering the 230-year-old Institute of Psychological Well being (IMH) in Chennai unexpectedly set the cat among the many pigeons. Within the first, Well being Secretary Supriya Sahu wrote to Director of Medical Schooling and Analysis J. Sangumani, expressing disappointment with the shortage of measures taken to enhance the residing circumstances of IMH residents, and ordered the implementation of sure selections already taken — modernisation of kitchen, budgetary allocation for meals, apparel and self-care equipment, an MoU between IMH and an NGO, further caretakers, and unbiased third-party analysis of IMH.
Within the second, she mentioned there was a necessity for institutional reforms to make IMH a premier establishment offering “gold requirements” of care. The institute has large alternatives to boost assets from nationwide and worldwide organisations in addition to from Company Social Accountability (CSR) funds, and desires steering from specialists working in psychological healthcare programmes, directors, and folks with intensive information within the discipline of therapy, care, rehabilitation, and integration of recovered sufferers with their households and communities. “It’s subsequently important that IMH is managed by a not-for-profit, wholly government-owned firm registered below Part 8 of the Firms Act. It will make sure that the federal government firm arrange may have the monetary and administrative flexibility and is ready to get the required experience from the board of the corporate.”
Over the times, nonetheless, this transfer got here to be interpreted because the State abdicating its accountability in the direction of its sufferers, {and professional} medical doctors’ our bodies expressed sturdy opposition.
Well being Division officers insist that the present scenario have to be seen as a chance to make clear the position of the varied actors within the psychological well being sector and transfer ahead sufficiently fortified to serve these with psychological sickness in the absolute best means — making certain therapy, human rights, continuum of care, and psychosocial rehabilitation. However detractors allege that the proposal will make IMH a “firm”.
‘State is accountable’
G.R. Ravindranath, normal secretary, Docs Affiliation for Social Equality, mentioned: “This stems from the Nationwide Psychological Well being Coverage that encourages public-private partnerships, utilising companies of civil society organisations and acquiring CSR funds. We aren’t opposing donations per se, however it’s the State’s accountability to establish the deficiencies and take measures to rectify them.”
The issue, nonetheless, won’t be solved with a number of donations, and on this occasion, the federal government doesn’t intend to surrender management over the establishment, as has been clarified a number of instances for the reason that controversy broke out. A senior official factors out that the Tamil Nadu Medical Companies Company Restricted (TNMSC), which has a streamlined process for drug procurement, storage, and distribution, was integrated below the Firms Act. It has since been capable of bail out the State throughout shortages within the Centre-supplied medicine, and has gained plaudits for its functioning. In truth, contesting the narrative that the State has abdicated its accountability, the official says the proposal would improve accountability and transparency and herald audits. In truth, the Particular Function Car envisaged on this case is a mannequin that brings in flexibility and the chance to faucet into funds. It helps in avoiding delays and motion will be fast in offering care, and positively it can’t be thought of privatisation. Responding to questions from mediapersons just lately, Well being Minister Ma. Subramanian mentioned the federal government would neither privatise IMH nor hand over its administration to an NGO.
R. Sathianathan, former director of IMH, factors out that for a number of years, funding was grossly insufficient and manpower was inadequate for IMH. He says the necessity of the hour is enchancment to its infrastructure and renovation of its wards.
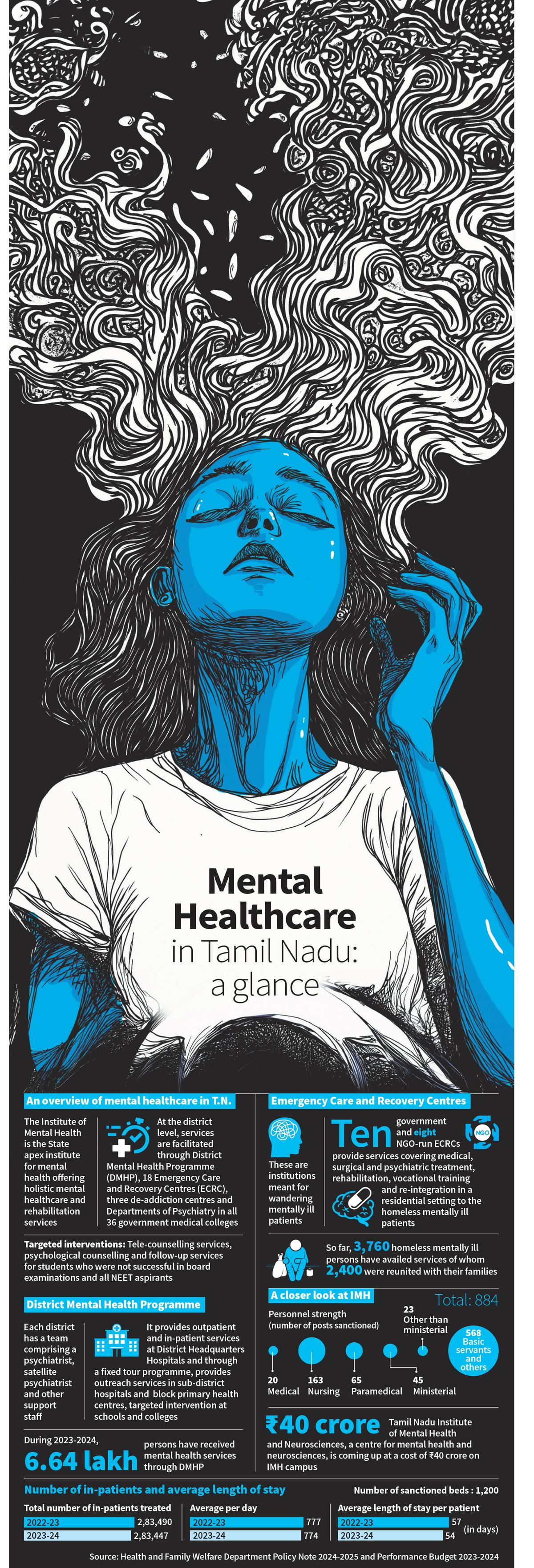
From a time when rescue and care of wandering mentally sick individuals had been tough owing to tedious processes, the State has come a great distance. It has simplified procedures to facilitate rescue and care of such individuals, P. Poorna Chandrika, professor of psychiatry and former director of IMH, factors out. “The institution of Emergency Care and Restoration Centres (ECRCs) has diminished the variety of homeless mentally sick individuals to an extent within the State,” she provides.
At IMH itself, therapy and rehabilitation has helped a variety of residents to be employed at varied locations; at the least 20 to 30 individuals have jobs now. Many IMH residents (who had been rescued as wandering mentally sick) have been reunited with their households in India and overseas. IMH Director M. Malaiappan says that on a median, 5,000 sufferers are admitted and an equal quantity are discharged from the institute yearly. “Now we have a system in place to hint and reunite sufferers with their households.”
Tamil Nadu has facilitated easy accessibility to psychological healthcare companies within the districts via the District Psychological Well being Programme (DMHP). “Tamil Nadu affords intensive psychological well being companies via DMHP clinics at authorities hospitals and block major well being centres (PHCs) throughout all districts. Over 600 authorities establishments supply psychiatry speciality outpatient division companies below the psychological well being programme frequently. The DMHP ensures sustainability, continuity, and complete psychological well being companies,” says R. Karthik Deivanayagam, Monitoring and Analysis Officer for Psychological Well being Programme, Tamil Nadu.
The DMHP has facilitated accessibility: DMHP satellite tv for pc clinics lengthen companies to all authorities hospitals and block PHCs, and screening, referral, and follow-up companies can be found from the PHCs, and common companies (outreach clinics) are offered on the premise of a set tour programme to make sure fixed-day companies at particular hospitals, he says. “The DMHP in Tamil Nadu has decentralised psychiatry companies, bringing them inside the attain of widespread man,” he provides. Important psychiatry medicine and speciality psychotropic medicine, together with clozapine, amisulpride, and olanzapine, are offered freed from price, enabling every household to save lots of ₹2,500 to ₹3,000 a month.
NGOs which were working in psychological well being for lengthy additionally acknowledge the DMHP’s attain. Vandana Gopikumar, co-founder, The Banyan, says the DMHP has penetrated the under-serviced areas; folks largely have entry to psychiatrists and psychotropic medicine. Nonetheless, the State ought to improve the variety of psychiatrists on responsibility, she provides.
Lakshmi Vijayakumar, psychiatrist and founder, SNEHA suicide prevention centre, says Tamil Nadu is without doubt one of the best-performing States within the DMHP below which each and every district has a psychiatrist and a social employee. So, the agricultural poor have higher entry to psychological healthcare companies. As compared with the opposite States, Tamil Nadu does have a psychiatry division in any respect authorities medical schools. At most establishments, the division has a mattress energy of 30, whereas smaller establishments have 10-20 beds.
Gaps in companies
R. Thara, vice-chair, Schizophrenia Analysis Basis, says psychological well being companies are much better in Tamil Nadu than in different States, particularly in north Indian States. “Now we have labored in States like Bihar the place there are districts with no psychiatrists. After all, there are nonetheless gaps in psychological healthcare in Tamil Nadu; many individuals requiring care will not be getting therapy. To enhance entry, the DMHP wants to coach PHC medical doctors in treating individuals with psychological sickness. Bigger PHCs will be outfitted with psychiatric medicines and coaching to cut back the hole,” she says. She pitches a separate cadre like Accredited Social Well being Activists for psychological healthcare for early detection and follow-up.
Employment alternatives for individuals with psychological well being points are nonetheless missing and insurance coverage doesn’t pay for psychological well being therapy, Dr. Lakshmi Vijayakumar provides.
A authorities psychiatrist acknowledges the shortfalls: “Drug shortages happen every now and then. Such shortfalls result in relapse in sufferers.” He provides, “What we want are midway houses and rehabilitation. The federal government ought to have a coverage to allow individuals with psychological diseases to take part within the workforce and company corporations ought to step in to supply employment. Now we have to simply accept the truth that a sure share of individuals have extreme psychological diseases and are tough to combine. Such individuals want long-term care.”
So far as the ECRCs are involved, continuum of care stays a query. One other authorities physician says, “Many are misplaced with out follow-up. There is no such thing as a mechanism to maintain monitor of sufferers. As well as, there isn’t a plan in place for social integration. Take this for example: at the least 5 to 6 sufferers proceed to remain for almost 1.5 years in one of many ECRCs.” Official sources underscore the necessity for added funding and human assets for the DMHP on the block degree, one counsellor per block, and an extra psychiatrist for the district headquarters hospital.
“Once we began within the Nineteen Nineties, psychological healthcare was sporadic and fragmented, and consciousness and entry had been minimal. We’re an conscious society now; nonetheless, prejudice and discrimination persist,” Ms. Gopikumar says. Strong integration of neighborhood inclusion into the care protocols will assist, she says. “Convergence between the well being and social sectors ought to be emphasised (with deal with incapacity allowance, housing, livelihoods) to deal with social determinants that impression psychological well being starting from poverty, violence, devaluation, grief, or intergenerational misery. Social staff and psychologists ought to be higher built-in into care programs to make sure adoption of value- and justice-based approaches. A cadre of psychological well being champions, who is perhaps lived-experience specialists or members of self-help teams and panchayats to kind neighbourhood solidarity networks that support disaster response and assist continuity of care, is necessary,” she provides.
Fostering collaboration
Tamil Nadu has finished effectively to foster a way of collaboration. The ECRCs are a working example. They’ve improved entry to applicable look after extremely susceptible teams, Ms. Gopikumar says, including: “The duty at hand is complicated and huge. To place the particular person with psychological sickness on the centre is vital: the State is the first stakeholder and accountable, and subsequently ought to nurture impactful and engaged partnerships. We have to encourage and encourage a tradition of collaboration and dialogue to make sure higher outcomes, particularly in an space fraught with inconsistencies and multifactorial causal pathways.”
Dr. Lakshmi Vijayakumar says the federal government has its personal equipment, whereas NGOs have their ears tuned extra to the bottom. They’re versatile, adaptable and reply sooner to the wants of the neighborhood. “We have to discover a seamless system whereby NGOs might be tasked to enhance consciousness and psychological well being literacy, establish and refer instances seamlessly to the well being system that treats the particular person, after which the particular person is introduced again to society for follow-up and rehabilitation. This shall be an ideal state of affairs for a affected person with psychological sickness,” she says.
Revealed – November 03, 2024 12:40 am IST