Scientists have created a brand new and extra superior type of immune-based most cancers remedy utilizing engineered cells generally known as CAR-NK (pure killer) cells. Like CAR-T cells, these modified immune cells will be programmed to acknowledge and assault most cancers, however they depend on a unique sort of immune cell that naturally targets irregular or contaminated cells.
A workforce from MIT and Harvard Medical College has now developed a more practical strategy to engineer CAR-NK cells that dramatically reduces the prospect of the physique’s immune system rejecting them. Immune rejection has been one of many greatest limitations of cell-based therapies, typically weakening their effectiveness.
This innovation might additionally make it doable to supply “off-the-shelf” CAR-NK remedies which might be obtainable instantly after prognosis, somewhat than ready weeks for custom-engineered cells. Conventional CAR-NK and CAR-T manufacturing strategies sometimes require a number of weeks to finish earlier than sufferers can start therapy.
“This permits us to do one-step engineering of CAR-NK cells that may keep away from rejection by host T cells and different immune cells. And, they kill most cancers cells higher and so they’re safer,” says Jianzhu Chen, an MIT professor of biology, a member of the Koch Institute for Integrative Most cancers Analysis, and one of many senior authors of the examine.
In exams utilizing mice with humanized immune programs, the newly engineered cells efficiently destroyed most most cancers cells whereas avoiding assault from the host’s personal immune defenses.
Rizwan Romee, an affiliate professor of medication at Harvard Medical College and Dana-Farber Most cancers Institute, can be a senior writer of the paper, which was revealed in Nature Communications. The examine’s lead writer is Fuguo Liu, a postdoctoral researcher on the Koch Institute and a analysis fellow at Dana-Farber.
Evading the immune system
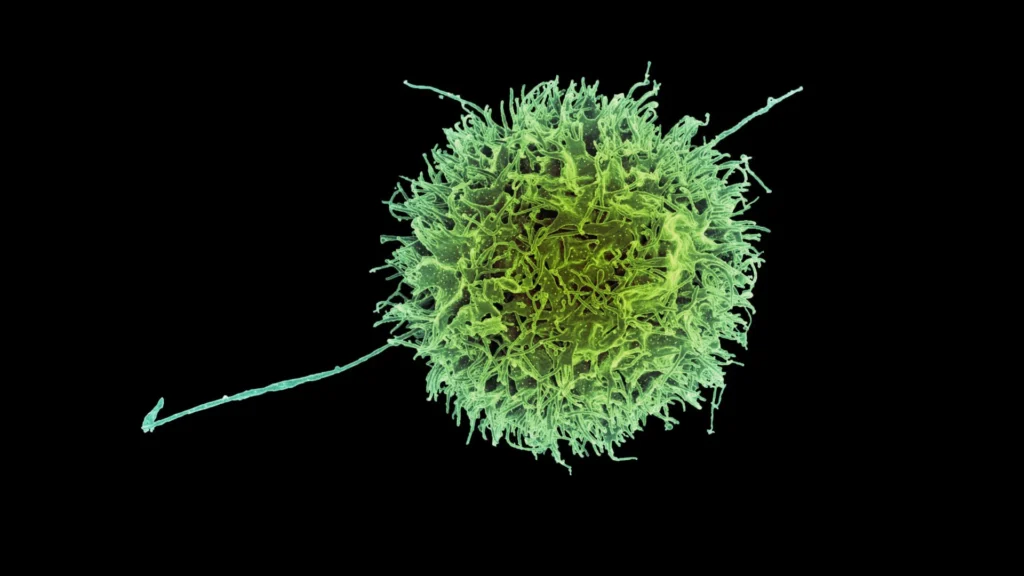
Pure killer (NK) cells are an important a part of the physique’s built-in immune protection, answerable for figuring out and destroying cancerous and virus-infected cells. They get rid of these threats by a course of known as degranulation, which releases a protein generally known as perforin. This protein punctures the membrane of goal cells, resulting in their loss of life.
To provide CAR-NK cells for therapy, medical doctors sometimes acquire a blood pattern from the affected person. NK cells are then extracted and engineered to precise a specialised protein known as a chimeric antigen receptor (CAR), which is designed to focus on particular markers discovered on most cancers cells.
As soon as modified, the cells should multiply within the lab for a number of weeks earlier than there are sufficient to be infused again into the affected person. The identical normal course of is used for CAR-T cell therapies, a few of which have already been authorized to deal with blood cancers like lymphoma and leukemia. CAR-NK therapies, nonetheless, are nonetheless being examined in scientific trials.
As a result of rising sufficient customized CAR-NK cells takes time and the affected person’s cells might not at all times be wholesome sufficient for dependable use, scientists have been exploring an alternate: creating NK cells from wholesome donors. These donor-derived cells could possibly be mass-produced and saved for fast use. The problem, nonetheless, is that the recipient’s immune system typically identifies donor cells as international and destroys them earlier than they will assault the most cancers.
Of their newest analysis, the MIT workforce aimed to unravel this drawback by serving to NK cells “disguise” from immune detection. Their experiments confirmed that eradicating floor proteins generally known as HLA class 1 molecules allowed NK cells to keep away from assault from T cells within the host’s immune system. These proteins usually act as identification markers that inform the immune system whether or not a cell belongs to the physique.
To utilize this perception, the researchers added a sequence of siRNA (quick interfering RNA) that silences the genes answerable for producing HLA class 1 proteins. Together with this genetic tweak, they launched the CAR gene itself and one other gene that encodes both PD-L1 or single-chain HLA-E (SCE), each of which assist strengthen the NK cells’ cancer-fighting skills.
All of those genetic parts have been mixed right into a single DNA assemble, which allowed the workforce to effectively convert donor NK cells into immune-evasive CAR-NK cells. Utilizing this technique, they engineered cells that focus on CD-19, a protein generally discovered on malignant B cells in lymphoma sufferers.
NK cells unleashed
The researchers examined these CAR-NK cells in mice with a human-like immune system. These mice have been additionally injected with lymphoma cells.
Mice that obtained CAR-NK cells with the brand new assemble maintained the NK cell inhabitants for at the least three weeks, and the NK cells have been capable of almost get rid of most cancers in these mice. In mice that obtained both NK cells with no genetic modifications or NK cells with solely the CAR gene, the host immune cells attacked the donor NK cells. In these mice, the NK cells died out inside two weeks, and the most cancers unfold unchecked.
The researchers additionally discovered that these engineered CAR-NK cells have been a lot much less prone to induce cytokine launch syndrome — a typical facet impact of immunotherapy remedies, which might trigger life-threatening problems.
Due to CAR-NK cells’ doubtlessly higher security profile, Chen anticipates that they may ultimately be used rather than CAR-T cells. For any CAR-NK cells that are actually in improvement to focus on lymphoma or different sorts of most cancers, it ought to be doable to adapt them by including the assemble developed on this examine, he says.
The researchers now hope to run a scientific trial of this method, working with colleagues at Dana-Farber. They’re additionally working with an area biotech firm to check CAR-NK cells to deal with lupus, an autoimmune dysfunction that causes the immune system to assault wholesome tissues and organs.
The analysis was funded, partly, by Skyline Therapeutics, the Koch Institute Frontier Analysis Program by the Kathy and Curt Marble Most cancers Analysis Fund and the Elisa Rah Memorial Fund, the Claudia Adams Barr Basis, and the Koch Institute Assist (core) Grant from the Nationwide Most cancers Institute.